CALL US: 818.605.4082
Email US: surgeon1936@yahoo.com
The Principles of Care
Any unwanted superficial vein, small or big, normal or varicose, is visible because they are located just under the skin and because dark colored blood flows in them. From practical point of view any cosmetically “unwanted” or diseased vein, can be treated by two basic modalities: removing them, or leaving them where they are, but closing them. Removing them is easy to understand as it implies a straight forward surgical procedure. Closing a vein, a tubular shaped blood vessel, by chemical ( sclerotherapy) or heat ( laser and radio frequency current-RF) is a more complex, more difficult and also more time consuming process, potentially also filled with several, occasionally severe complications I personally dislike and therefore do not use in my setup. Closing methods are based on the principle that any organ/tissue, when injured, will mount an inflammatory reaction that, in the end, will heal the injury by generating a scar tissue serving as a glue. In case of veins, this scar tissue is expected to close/obliterate the vein. Once flow of blood in the (closed) vein becomes impossible, the vein becomes invisible and if symptoms were present, they should disappear.
The interested reader should know that there are "stiff" hemodynamic principles that all therapeutic options will have to follow in order to achieve the best cosmetic, functional as well as best lasting result, knowing that varicose veins can be a recurring condition. The minimally invasive new surgical protocol (ambulatory phlebectomy) is the best as the method follows closely these principles thus will yield the best results. I am sorry that it may not be easy to understand the following sentences, however, I will try to do my best...
Varicose vein, a disease of the superficial venous system, is characterized by a weakness of the vein wall causing vein distention i.e. dilatation. Once distended /dilated, most valves, existing along the diseased vein meant to assure the uphill physiologic flow, will become incompetent. This means: they will leak (in standing position) and the normal physiologic uphill -back to heart - blood flow, will reverse course (with the help of gravity), and become a downhill flow, back to calf and ankle. This blood flow pattern is called reflux. That is the scenario only if the patient is upright on his/her feet. With patient recumbent, even better with elevated leg, the favorable gravitational forces, will automatically facilitate decongestion of all veins with resumption of the normal uphill back-to-the-heart flow. (One can easily understand now the beneficial effect of leg elevation. If you have varicose veins, please lie down and elevate your leg; all bulging veins will disappear in seconds, but the moment you resume an upright position, the veins will fill up in just several seconds...
To make all this and the following sentences easier to understand, let's imagine an overflowing, dripping an existing higher above the ground water faucet, you or the gardener attaches the hose to watering the lawn or flowers. Obviously, aided by gravity, the dripping water will be sooner or later flooding the ground and with passage of time it will create a paddle. Yes, the gardener could cover the puddle with sand, gravel or any other type of fill, however, as long the leaking faucet is not properly controlled/fixed this will be a futile exercise. Only properly addressing the faulty faucet will the wet ground dry up and stay dry.
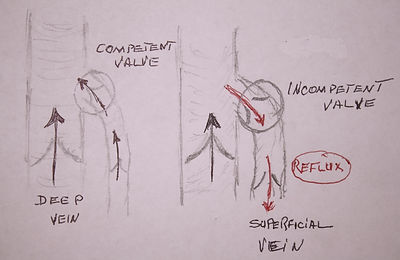
Fig. 1 Normal (uphill) and pathological (downhill) flow at the groin junction between the superficial long saphenous vein and femoral vein.
Truncal varicose veins (VV) present a very similar - just described - scenario. The "faucet" or as we doctors call it, "escape point" is not visible and we will have to use an ultrasound examination to localize it. Along the entire leg - in overwhelming cases - the "escape point" is only in two anatomic places: either in the groin or behind the knee. In these two fix anatomical places, leg’s superficial vein (called saphenous) will join deep veins (femoral vein in the groin and popliteal vein behind the knee), sites called junctions; (SFJ for saphenofemoral in the groin and SPJ for sapheno-popliteal behind the knee). These two junctions are normally protected by a major valve responsible for maintaining the normal back-to-the-heart, uphill flow and never enable reversed downhill flow from the much larger deep veins in to the superficial leg veins. Therefore, as long as this valve is competent i.e. normal, in no circumstances blood, from the larger deep vein can spill into the easily distensible superficial veins. Never! However, in the presence of a leaky i.e. incompetent junctional valve, blood from the deep vein, helped by gravity, (like water in the presence of an overflowing faucet mentioned above), will escape into the superficial veins and will start its journey in an reversed, downhill fashion, (flow pattern called reflux) that will not just create but also sustain the superficial varicose veins and make them even worse with passage of time. The distended bulging, tortuous veins at the beginning will create only cosmetic distress but with passage of time, venous pressure rises too, and the patient may become symptomatic complaining of discomfort, pain, ankle swelling. Later complications such as superficial phlebitis, chronic venous insufficiency, venous ulcers may occur too.
The main difference between the two scenarios is that water flooding the ground is a free-fall fashion, while blood, in its downhill/reversed course, uses as a conduit, the existing axial superficial vein trunk (axial conduit or vein) extending from the groin junction to inner aspect of ankle (the long saphenous vein) or from behind the knee junction to the lateral aspect of ankle (the short saphenous vein).
This conduit, in normal physiologic conditions, collects uphill flowing blood through attached branches/tributaries existing along the entire leg. In varicose veins, as previously mentioned, flow is reversed i.e. downhill, from the axial vein into the branches or tributaries. In most cases, as positioned in slightly deeper structures of the thigh and calf, this axial vein is not visible but we can map it out with ultrasound easily. (For more detailed information please read anatomy and physiology.)
To achieve the best therapeutic result, any treatment modality available for varicose veins has to follow three major steps. (See drawing).
Step 1. The method has to completely close/obliterate/stop the leakage of blood originating at the level of the escape points/junction, groin or behind the knee or both (rare occasions).
Step 2. The method has to also stop (remove or close) the downhill pattern of blood flow existing in one of the axial saphenous vein trunks that permits large volumes of blood to spill/”flood” the thigh or calf branches/tributaries of the axial vein causing them further to distend and bulge.
Step 3. The method lastly, should also take care of the distended and bulging tributaries either removing or closing them, preferably in the same session.
Removing a vein is straightforward, either the traditional and by now obsolete traumatic stripping and the minimally invasive Ambulatory Phlebectomy.
Closing a vein is possible by either chemical injury i.e. injection sclerotherapy or by thermal injury the endovenous thermal ablation by laser or RF current.
The methods linked to the closure option are plagued with problems and unnecessary complications, some of them, such as thromboembolic ones, potentially lethal. Should you opt for any of these options you will have to sign a consent form and all these complications will be clearly mentioned.
The common problems encountered with vein closure methods are that neither Step 1 nor Step 2 can be properly implemented and the control of the reversed flow/reflux will not be complete. The reason for all this is in obligatory blood clot formation after any form of vein injury. This is an innate physiological defense mechanism meant to stop bleeding in an injured vein. If clot formation would happen at the site of the escape point/junction, a place were the superficial axial vein trunk dead-ends in the deep vein, the"simplest complication" possible would be a deep vein (iliofemoral) thrombosis or DVT, a quite terrible condition when the leg will blow up resembling an elephant's leg. This could mean at best just hospitalization and long-term anticoagulation i.e. blood-thinning medication. Please remember, once you had a blood clot in a deep vein, the chances of getting another one in course of your life, are much increased. Should, however, the clot break up and enter the circulation, it could end lodging into the lungs causing pulmonary emboli or PE which, if massive, could be even lethal. To try preventing all this to happen all methods aimed to close a vein will not go all the way up to the level of the escape point but will stop just below the actual escape point/junction by at least 2-3 cm. This will obviously short changes Step 1. meant the hermetically control the escape point and prevent blood from escaping and starting it's downhill/reversed pattern of reflux flow. A clot is formed without exception in the axial vein trunk too, this can short change Step 2 by preventing a proper closure of the axial vein conduit by lack of a proper scar formation. Moreover, physiologically any formed clot shrink, even melt and if this happens the axial vein was never properly closed or will reopen at a later date permitting the resumption of the downward reflux flow. The reestablished reversed pattern of blood flow (reflux) will fill up old/new branches that with the passage of time will bulge and distend. If this happens weeks or just a few months after the procedure, we have immediate failures. If it happens later, they are considered late failures.
Taking in account all of the above, without a shadow of a doubt, the safest and the best way to treat truncal varicose veins is using surgery, the only modality capable to deliver full control of the Steps (1-2-3) enumerated above, essential steps to achieving maximal results with minimal complications. Using the full ambulatory phlebectomy protocol enables the performance of this minimally invasive surgical protocol also in an office setting and local anesthesia, contradicting the vein closure advocates (industry and physicians) who trumpet the misleading concept that any form of varicose vein surgery always necessitates general anesthesia, always has to be performed in hospital/surgicenter setting, is always traumatic, always needing long convalescence and loss of income. What a farce!
A side note:
A word of caution, an ultrasound examination is mandatory to properly map the position of the escape point in the groin or behind the knee (Step 1) and the axial vein paying attention also to the extent of reversed (reflux) pattern of flow (Step 2). This examination is preferably performed by the practitioner responsible for the results. While there are older methods in achieving a proper clinical diagnosis there is no excuse not to be examined at least by an auditory Doppler ultrasound. Of course, a duplex ultrasound imaging is much better. Ultrasound examinations have to be done standing as the reversal of flow (reflux) existing in varicose veins is gravitationally induced. If therapeutic conclusions were obtained from a duplex imaging test performed just lying down, please change the practitioner. In case the test is done in a Radiology suite, the practitioner should preferably be present at the time of the examination.

Truncal Varicose Veins:
Principals of care.
(Click to enlarge)
