CALL US: 818.605.4082
Email US: surgeon1936@yahoo.com
Final Conclusion
A patient seeking help for existing varicose veins is interested in symptom (pain, swelling, etc) relief and cosmetic relief.
Varicose vein, a disease of the superficial venous system, is characterized by a weakness of the vein wall causing vein distention/dilatation. Once distended /dilated, most valves, along the diseased vein, will become incompetent. This means: they will leak and the normal uphill - back to heart - blood flow, with the help of gravity, will reverse course and become a downhill flow, back to calf/ankle. This flow pattern is called reflux. That is the scenario only if the patient is upright on his/her feet. With patient recumbent, even better with elevated leg, the favorable gravitational forces, will automatically facilitate resumption of the normal uphill back-to-the-heart flow. (One can easily understand now the temporary, but beneficial effect of leg elevation.)
To make all this and the following sentences easier to understand, let's imagine an overflowing faucet. Obviously the escaped water, aided by (the same) gravity, in a free fall fashion, will be flooding the floor. Once leaking faucet is fixed and overflow properly controlled, future flooding should be prevented.
Truncal varicose veins (VV) present a very similar scenario. The "faucet"/escape point is, however, located either in the groin or behind the knee, places were leg’s superficial vein (called saphenous) will join deep veins (femoral in the groin; popliteal behind the knee), sites called junctions (SFJ respectively SPJ). These two junctions are normally protected by a major valve responsible not just for maintaining the normal back-to-the-heart, uphill flow but also to drain the blood from the superficial system into the deep. Therefore, as long as this valve is competent i.e. normal, in no circumstances blood, from the larger deep vein can spill into the superficial vein. Never! However, in the presence of a leaky i.e. incompetent junctional valve, blood from the deep vein, helped by gravity, (like the water in the presence of an overflowing faucet mentioned above), will escape into the superficial vein and will start its journey in an reversed, downhill fashion, flow pattern called reflux (Fig. 1).
Obviously, blood will not be “flooding" floors, but disease affected and already distended, bulging branches/tributaries of the vein that caused patient’s cosmetic distress in the first place. If, with passage of time venous pressure rises too, the patient may become symptomatic complaining of discomfort, pain, ankle swelling and complications such as superficial phlebitis, chronic venous insufficiency, venous ulcers may occur.
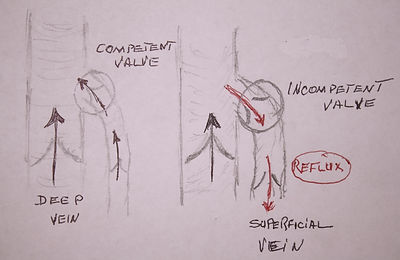
Fig. 1 Normal (uphill) and pathological (downhill) flow at the groin junction between the superficial long saphenous vein and femoral vein.

Truncal Varicose Veins:
Principals of care.
(Click to enlarge)
The main difference between the two scenarios is that water flooded the floor in a free fall fashion, while blood, in its downhill/reversed course, uses as a conduit, the existing axial superficial vein trunk extending from the groin junction to ankle (the long saphenous vein) or from behind the knee junction to the ankle (the short saphenous vein). This conduit, in normal physiologic conditions, collects uphill flowing blood through attached branches/tributaries existing along the entire leg. In varicose veins, as previously mentioned, flow is reversed i.e. downhill, from the axial vein into the branches/tributaries (Fig. 2). Positioned in slightly deeper structures of the thigh and calf, in most cases, this axial vein is not visible. (For more detailed information please read anatomy and physiology.)
To achieve the best therapeutic result, any treatment modality available for varicose veins has to follow three major steps. (See drawing).
Step 1. The method has to completely close/obliterate/stop the leakage of blood originating at the level of the escape point/junction regardless its position : groin or behind the knee.
Step 2. The method has to also stop (remove or close) the downhill pattern of blood flow existing in the saphenous vein trunk (either along the inner aspect of the thigh or along the hind side of the calf) being the axial conduit enabling the downhill/reversed pattern of flow ("reflux"), and permitting large volumes of blood to spill/”flood” the branches/tributaries of the axial vein, causing them further to distend/bulge.
Step 3. The method lastly, should also take care of the distended and bulging tributaries either removing or closing them, and if just possible, in the same session.
Presently, there are several therapeutic modalities available to choose from. Personally I am also guided by additional practical principles:
-
Method to be minimally invasive and performable in an office setting and local anesthesia if necessary.
-
Method to offer results in the shortest period of time,
-
Method to offer long lasting results in a condition were recurrences are the rule rather than exception,
-
Method to have low morbidity, i.e. minimal if any local or distant complication and never subject/expose a varicose veins patient (basically a cosmetic condition) to the potentially life threatening venous thromboembolism such as deep vein clot (DVT) and pulmonary emboli (PE).
-
Method to be cost efficient.
Injection sclerotherapy in all of its forms: liquid or foam/froth, ultrasound guided is an office procedure, but is potentially requiring multiple treatment sessions and is associated, in most cases, with an inconvenient and lengthy compression protocol meant to prevent blood clot formation. Local complications (skin pigmentation and ulceration) are quite frequent, distant complication such as deep vein thrombosis (DVT) and (potentially) life threatening pulmonary emboli (PE) have been reported not to speak of the systemic complication (mainly associated with foamed solution) such as confusional states, transient blindness and limb paralysis due to micro air emboli.
The reported high immediate failure rates (up to 10%!) should be unacceptable if critical review of results is implemented. Could anyone imagine being suggested a therapeutic modality for removing a gallbladder that fails in up to 10% of cases? Indeed, out of 100 patients undergoing the procedure, in 10 (!!) the gallbladder would be left behind; not that it grew back... was left behind!!
There are two reasons why injection sclerotherapy may fail in such significant numbers is because the above described Step 1 and Step 2 are difficult to execute properly. The problems in executing Step 1 is because injections are stopped 2-3 cm below the actual "escape point" (the junction between the superficial and deep veins) from fear that the induced blood clot may extend into the deep veins causing a deep vein thrombosis, DVT or, should the clot break up and fly upward in the deep vein circulation it may lodge itself in the lungs causing pulmonary emboli, PE, a potentially lethal condition. The problems with Step 2, causing the high immediate (weeks/months) as well as late failure rates, is explained by the inability of the method to properly control the reversed pattern of flow existing in the axial vein as the method can't properly prevent blood clot formation in the injected veins not even with best of a compression protocol meant to prevent it. Any formed blood clot is the biggest enemy for a proper scar formation necessary to close the vein, besides, that a clot will always retract with passage of time, basically "melt" (a normal physiologic process) thus enabling resumption of the reversed and downhill pattern of blood flow (reflux) in the axial vein and renewing the distention/ bulging of the branches like nothing happened!
In conclusion, injection sclerotherapy is not the best therapeutic modality for the full fledged truncal varicose veins if one takes in consideration the immediate and late high recurrence rates and if one also takes in consideration the existing potential for disastrous complications DVT and PE mentioned above. Indeed, in a recent European multi-center study of 500 consecutive cases comparing all three therapeutic modalities available for varicose veins (sclerotherapy, endovenous ablation and surgery), foam sclerotherapy came the least good having a 17.1% failure rate after just a single one year follow up. In simple translation, in the first year after the procedure, 17 patients out of 100 remained... were not cured. Time and money (for vein) was spent in... vain. It had also the highest complication rate including DVT and PE. The method is however, useful for minimal branch varicosities, residual vein after surgery or after endovenous ablation or in too small veins not amenable for removal by ambulatory phlebectomy and of course spider veins.
Endovenous thermal ablation is also performed in an office setting and is meant to achieve vein closure this time by delivering (not chemical but) heat injury (via a catheters/probes placed - also under ultrasound guidance - in the vein) to the inner lining of the vein wall which is in principle is similar to the chemical injury seen with sclerotherapy. There is however a major difference as the generated effective heat - just below water’s boiling point (85º-90º) - by altering the collagen fibers structure existing in the vein wall - shrinks the vein almost instantaneously as the catheter is slowly removed. There are basically two modalities that use this principle:
A. Endovenous radio-frequency (RF) ablation, ERFA or RFA formerly also known as VNUS or Closure, using heat generated by radio-frequency (RF) current/energy and
B. Endovenous laser ablation, EVLA or simply ELA (also known as EVLT) that is using lasers targeting the red cell's hemoglobin to generate hot steam that in turn will cause the needed injury to the same inner lining of the vein as well as vein wall identical with RF ablation.
These two heat injury alternatives, are in effect in the same boat with injection sclerotherapy (problems mainly with step Step 1 and possibly with Step 2) having also a relatively high immediate as well as late failure rates besides the same potentially dire thromboembolic consequences. The reasons are identical with the ones enumerated with injection sclerotherapy. None of these two endovenous heat alternatives can properly occlude the proximal escape point as they too stop short of the actual escape point having the same fear of generating a blood clot able to propagate into the deep system causing "at best" just DVT, and at worst PE. Should the patient end up having "just" a deep vein clot (DVT) he/she may still end up in a hospital and also be submitted to a lengthy blood thinning therapeutic protocol. Moreover, once one had a deep vein clot, the chances having another in course of a lifetime is much increased. If, however, the deep vein clot ends up in the lungs (PE) this could potentially represent a lethal complication. As I have mentioned before, I can't embrace and certainly perform any procedure - for basically a cosmetic condition as Varicose Veins indeed are - while exposing the patient to potentially disastrous/catastrophic complications. Not as long as I live and practice medicine.
The methods, I read, have also a more rough immediate postoperative course with oozing of the generous amount anesthetic solution, used in tumescent anesthesia, needed to isolate surrounding tissue such as skin and nerves protecting them for being burned during the process of injuring the vein with temperatures just below boiling point. Other local complications were excessive pain due to deep tissues blood collections (hematoma), indurated skin due to explosive perforation of the treated axial veins, etc.etc.
Stripping surgery in its traditional approach, from medical point of view rids the patient of all diseased veins perfectly, but the frequent nerve injury caused by the oversized stripper head, the excessive tissue trauma, the generous and ugly crisscrossing scars that were the rule rather than the exception, the weeks of convalescence and loss of income, the need for hospital setting and general anesthesia made this procedure by now OBSOLETE, especially in today's medical/surgical environment dominated by minimally invasive procedures.
Fig. 3 Peeling a banana: inside skin becomes the outside...
Ambulatory Phlebectomy (AP) is indeed the minimally invasive surgical alternative for the traditional traumatic stripping, exactly as today’s laparoscopic gallbladder surgery is for the old and traditional open cholecystectomy. AP contrary to the brain washed public's belief that all surgery needs hospital setting and general anesthesia - is performable in an office setting and simple local anesthesia. Step 1, control of the escape point is taken care by a direct vision open approach through a 2 inch groin incision that enables maximal control of the escape point be it in the groin or behind the knee. AP incorporating the tamed “peel-out” - PIN (perforate invaginate) stripping of the axial vein in its protocol totally controls the axial reflux (Step 2) harboring the downhill pattern of flow. The "peel-out" removal of the axial vein is totally atraumatic much different than the traditional stripping that used a large stripper head that literally ripped out the vein causing severe soft tissue trauma. Please imagine peeling a banana (Fig. 3) as the inside of its skin is turning to be... outside, or for the matter removing a glove from the hand it covered (Fig. 4-5). The side of the glove that was in contact with hand's skin will turn to be outside...so is the vein, when removed: the inner lining is on the outside and the outside lining becomes... the inside one. Each leg is operated in one single session, branches/tributaries included (Step 3) via 1-3 mm skin opening using the available mini hooks.
The entire AP protocol in our setup is performed in local (femoral block) anesthesia for the long saphenous vein and infiltrative local anesthesia for all the branches as well as the short saphenous vein. Pain is minimal; most patients do not need any form of medication, OTC drugs included. Bruising is possible but will disappear in 1-2 weeks. Return to daily activities including sporting activities (except swimming) is immediate. Patients who opted not to have a tranquilizer, drive themselves away from the office. No superficial phlebitis or deep vein thrombosis (DVT) has been observed in 3500 plus operations. No immediate failure has been ever observed as veins are removed and not challenged to stay where they are, yet close. The cosmetic results - with no left over visible scars, no skin ulcers or pigmentation - are excellent surpassing all other enumerated modalities (See link).
In conclusion, taking in account all of the above, without shadow of a doubt, the safest and the best way to treat truncal varicose veins is using surgery, the only modality capable to deliver full control of the Steps (1-2-3) enumerated above, essential steps to fully control the reversed pattern of flow and by this achieving maximal results with minimal complications. Using the full ambulatory phlebectomy protocol enables the performance of this minimally invasive surgical protocol also in an office setting and local anesthesia, contradicting the vein closure advocates who trumpet the misleading concept that any form of varicose vein surgery always necessitates general anesthesia, always has to be performed in hospital/surgicenter setting , is always traumatic, always needing long convalescence and loss of income. This is how the benefits of any of these closure methods (injection sclerotherapy and thermal ablations) as the only "in office" varicose veins treatments are promoted, options as we have seen are much less good and with increased chances for potential complications, inclusive dreaded thromboembolic ones. Let's not forget that ambulatory phlebectomy is from A-Z completely surgeon dependent who removes the veins, whereas any of the closure method keeps the vein in its place but trying to close it, a much more difficult achievable task.


Fig. 4 Removing/peeling off a glove: the inside of the glove in contact with the hand's skin becomes the outside in an easy maneuver too...

Fig. 5 Idem, removing of a glove
It is unfortunate that AP as performed in an office setting and local anesthesia is still sitting on the side lines. It is also sad that my surgeon colleagues have let me (and the procedure) down. One of the main reason being that traditionally, surgeons were disinterested in varicose veins as they considered the condition just a cosmetic nuisance, not a disease. Secondly, if one is a provider for insurance carriers - which I am not - reimbursement at least here in the US favors high tech procedures and works against surgery of any kind. In a document in my possession received from VNUS technologies manufacturer of hardware for RF ablation trying to entice me to join the crowd, which obviously I did not, the 2009 Medicare National Payment Rates says it clearly: for a "45 minutes" high tech RF ablation (ClOSURE) procedural (CPT) code 36475 was reimbursed (in 2009) for $ 2,493!! whereas for a vein stripping surgery (CPT code 37722) a provider would get a meager... $ 465! You decide which procedure is preferred...I am also aware that operating in a general anesthesia is more surgeon friendly than using local anesthesia. A London story comes into my mind..."Stanley", I said while watching him operate on a Saudi Prince with huge varicose vein in of course private hospital, "I do the entire minimally invasive protocol in an office setting and local anesthesia", to which, after he elevated his rich and bushy dark, dark eyebrows he said in a loud and quite angry voice: "Whaaat? Do I also have to entertain the patient?" Oh, yes, surgeon's well known commodity...
I am therefore among the few, if not the only one, left to stand the ground and fight for the recognition of the minimally invasive protocol as the best and least dangerous approach available to treat truncal varicose veins and I do not mind being considered, or reminded by some, being... Don Quixote de la Mancha basically fighting the “windmills”... I sleep well and my patients are mostly happy as... indeed, I am better than most, not as good as...(few) some...
The lone fighter

